Focus: Ensure fetal surgery safety

Detailed surgical planning, operative checklists and multidisciplinary care coordination are critical for the safety of fetal surgery. The surgery, performed only for conditions that can be fatal or can progress in utero causing harm that cannot be surgically reversed after birth, is offered in only about a dozen pediatric medical centers nationwide.
St. Louis Children’s Hospital started its program in August 2017, filling a much-needed niche in the central Midwest region. Headed by pediatric surgeon Jesse Vrecenak, MD, and Pediatric Surgery Chief Brad Warner, MD, the Jessie L. Ternberg, MD, PhD Distinguished Professor of Pediatric Surgery, the team has worked carefully to ensure safe practices.
Vrecenak joined St. Louis Children’s after completing a fellowship under N. Scott Adzick, MD, surgeon-in-chief at The Children’s Hospital of Philadelphia and a pioneer in fetal surgery. “Dr. Adzick operates with machine-like precision,” says Vrecenak. “The surgery is all about efficiency, economy of movement, and making sure all the moving parts fit together seamlessly.”
Vrecenak, under the direction of Warner, is working with pediatric neurosurgeons to treat myelomeningocele, a spine defect that is the most serious form of spina bifida. Babies with spina bifida are at high risk for developing hydrocephalus, or fluid build-up within the brain. Fetal surgery to close the spine significantly decreases this risk. Affected patients also can experience varying degrees of leg paralysis, but surgery before birth can provide better lower extremity function, doubling the likelihood a child will walk independently.
With close collaboration and attention to detail, fetal myelomeningocele repair can be performed safely. In addition to surgeons, non-surgical specialists on the team include: anesthesiologists, maternal fetal medicine specialists, sonographers, fetal cardiologists, neonatologists and extensively trained scrub nurses.
Initial surgical outcomes are good, and the program shares its results with other centers through the NAFTNet Fetal Myelomeningocele Consortium.
Open fetal surgical intervention can treat far more rare birth defects, including lung lesions compressing the heart and tumors around the heart that would result in heart failure in utero or after birth if left untreated. The key, says Vrecenak, is to safely perform the procedure to minimize the risk of premature birth as a result of the intervention.
“Prematurity is the Achilles heel of fetal intervention,” says Vrecenak. “We want every mom to get to 37 weeks.”
Highlights
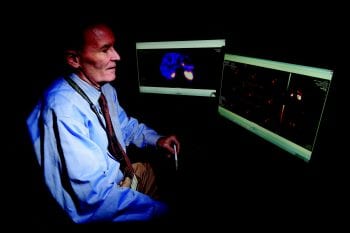
A congenital hyperinsulinism center of excellence is being established at St. Louis Children’s Hospital. The multidisciplinary program, which will be the largest such program in the central Midwest, includes surgeon Patrick Dillon, MD, and pediatric specialists in endocrinology, nuclear medicine, neonatology and pathology. Congenital hyperinsulinism is a rare condition caused by overactivity of beta cells in the pancreas, which over-secrete insulin and make newborns hypoglycemic, lowering their blood sugar. If the hypoglycemia reaches a critically low level, it can cause seizures, developmental delays and other major health issues. At St. Louis Children’s, the condition is treated either medically or surgically based on response to medication, genetics and results of positron emission tomography–magnetic resonance imaging (PET/DOPA-MRI), utilizing a special isotope.
Kristin Seiler, MD, a Washington University general surgery resident, received a resident research award from the Association for Academic Surgery and funding through the Children’s Discovery Institute for her research conducted in the Intestinal Adaptation Laboratory. She researches how the development of small blood vessels impacts cell growth and wound healing as well as how to build an appropriate acellular scaffold to grow tissue-engineered small intestine.
Cathleen Courtney, MD, was awarded the Marion and Van Lear Black Fellowship in Pediatric Surgery. Courtney, a Washington University general surgery resident in the Intestinal Adaptation Laboratory, studies the metabolic consequences of massive bowel resection, including fatty liver disease, glucose intolerance and enlargement of the pancreas.