Focus: Evaluate new devices for heart and valve diseases

Heart surgeons in the Washington University and Barnes-Jewish Heart & Vascular Center are leaders in testing new technology to improve outcomes and safety in patients with heart valve disease and heart failure. This opens up treatment options for patients who cannot undergo valve surgery safely and improves survival and quality of life for patients whose hearts need mechanical support as a bridge to transplant or permanently.
The center was a leading enroller in the PARTNER (Placement of AoRTic traNscathetER) trials, which tested transcatheter aortic valve replacement (TAVR) in patients with narrowed aortic valves. Surgeons and cardiologists implant the new valve by threading a catheter from the femoral artery in the leg to the heart. TAVR is now Food and Drug Administration-approved for inoperable, moderate and high-risk patients. The final low-risk trial just concluded.
“Almost all patients can be treated with transcatheter procedures or open surgery,” says heart surgeon Hersh Maniar, MD, co-principal investigator of the last three PARTNER trials along with cardiologist Alan Zajarias, MD. “It requires nuanced selection according to anatomy and other patient characteristics.” Several surgeons, including Spencer Melby, MD, and Puja Kachroo, MD, now participate in all TAVR procedures.
Transcatheter mitral valve replacement is also being tested in clinical trials, which Maniar and Melby lead along with Zajarias and cardiologist John Lasala, MD.
In heart failure patients, left ventricular assist devices (LVADs) provide mechanical circulatory support to pump the heart until a heart transplant is available or as destination therapy in patients who aren’t eligible for transplant. Two-year survival rates have risen dramatically since the 1990s, when the HeartMate XVE had an approximate 40 to 50 percent two-year survival. Next generation models, HeartMate II and HeartWare, improved the survival rate to 71 percent.*
The Heart Failure Program was one of five centers in the country to start the investigation device exemption (IDE) Momentum Trial for the latest model, HeartMate 3, now approved as a bridge to transplant and destination therapy. Heart surgeon Akinobu Itoh, MD, PhD, was site principal investigator of the device’s destination therapy trial. A New England Journal of Medicine study found the HeartMate 3 had a two-year survival rate of 82.8 percent.†
Technology such as HeartMate 3’s magnetically levitated cardiac pump has “dramatically improved pump thrombosis rate,” says Itoh.
*Prinzing A, Herold U, Berkefeld A, Krane M, Lange R, Voss B. Left ventricular assist devices—current state and perspectives. Journal of Thoracic Disease. 2016;8(8):E660-E666. doi:10.21037/jtd.2016.07.13.
†Mehra MR, et al., for the MOMENTUM 3 Investigators. Two-Year Outcomes with a Magnetically Levitated Cardiac Pump in Heart Failure. N Engl J Med 2018; 378:1386-1395.
Highlights
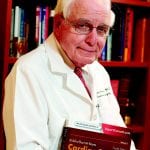
Nicholas Kouchoukos, MD, is the first John M. Shoenberg Emeritus Chair of Cardiothoracic Surgery, recognizing his leadership in the field. He has spent 44 combined years with BJC HealthCare and Washington University School of Medicine, serving as surgeon-in-chief at Jewish Hospital from 1984 to 1996. A graduate of Washington University School of Medicine and its general surgery residency program, Kouchoukos also edited “Cardiac Surgery,” a definitive textbook in the field.
Cardiothoracic Surgery Division Chief Ralph Damiano Jr., MD, Research Professor Richard Schuessler, PhD, Cardiac Surgery Section Chief Marc Moon, MD, and colleagues retrospectively studied almost 11,000 patients who underwent cardiac surgery at Barnes-Jewish Hospital to see if surgically treating their atrial fibrillation (AF) in the same operation as another heart condition produced better outcomes. The researchers studied three groups: patients with a history of AF who received a Cox-Maze IV procedure in the same operation (using radiofrequency ablation to restore sinus rhythm); patients with AF not treated for the condition during surgery; and patients without AF. Patients who had Maze and heart surgery had a 10-year survival rate of 62 percent, the same as for patients without AF. AF patients who were only treated for another heart problem had a 42 percent 10-year survival. The research was published in the Journal of Thoracic and Cardiovascular Surgery. The National Institutes of Health has funded the division’s AF research for 34 consecutive years.