Focus: Cut the weekend readmissions rate

In just one year, the Division of Urologic Surgery saw a dramatic drop in the readmissions rate of patients initially discharged on a weekend.
“The Department of Surgery overall has improved its readmission rates, but one of our division’s efforts focused specifically on readmissions after weekend discharges, which are historically high,” says Urologic Surgery Chief Gerald Andriole, MD, the Robert K. Royce Distinguished Professor of Urologic Surgery.
A team led by urologist Erica Traxel, MD, and Chief Resident Joseph Song, MD, studied the “weekend effect” shown in data collected for the division by Vizient, a management consulting firm. During the first 11 months of 2016, urology patients discharged on the weekend had a 13.8 percent chance of being readmitted compared to a 7 percent rate for weekday discharges. Those discharged over the weekend did not appear to have greater risk factors for readmission such as severity of illness or being admitted through the ICU.
The team educated residents and faculty and then implemented a discharge checklist covering procedures such as examining drains/catheters and educating patients on wound care. In 10 months after implementation, patients discharged during weekends had only a 3.8 percent readmission rate, compared to a 5.7 percent rate on weekdays.
Reducing unavoidable hospital readmissions is critical to improve patient safety, enhance quality of care and lower health care spending. Hospitals began voluntarily reporting hospital readmission rates to the Centers for Medicare & Medicaid Services (CMS) in 2009. In 2012, the CMS took a step further by reducing Medicare payments for hospitals with excessive rates of 30-day readmissions for some conditions and treatments.
Washington University urologists face special challenges at Barnes-Jewish Hospital because it is a teaching hospital and has a higher share of low-income patients; these factors were shown to increase patients going back to the hospital within 30 days under CMS’ readmission reduction plan. Although Congress enacted legislation to make a socioeconomic adjustment in Medicare payments to these hospitals, the Division of Urology continued to work on steps to reduce its readmission rates.
The results of the “weekend effect” project were presented in October at the 2018 Vizient Fall Connections Summit.
Highlights
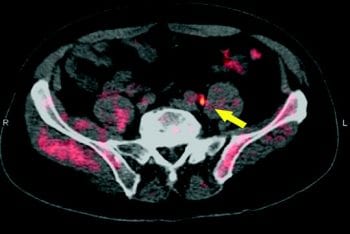
Urologic Surgery Division Chief Gerald Andriole, MD, led the LOCATE national clinical trial that demonstrated the effectiveness of using the radiotracer 18F-fluciclovine with a positron emission tomography (PET) scan to identify and more accurately target locations of recurrent prostate cancer. A radiotracer is a radioactive substance that produces images of an organ or tissue that can be seen on a PET scan. Previously, there was no scientific way to determine the location of the recurrent cancer. In the study, clinical management changed in 59 percent of patients when PET/CT results were added to the diagnostic work-up. Of those changes, 78 percent were classified as “major,” indicating a change in treatment modality.
The urologic surgery residency program expanded from three to four interns this year. The expansion supports three urologists at Christian Hospital, who have a burgeoning practice and who also provide care at Siteman Cancer Center-North County, which opened in 2017. Urology residents treat a volume and diversity of surgical cases that are among the highest for urologic residencies in the country.
Prostate cancer researchers Nupam Mahajan, PhD, and Kiran Mahajan, PhD, joined the division in August 2018. Nupam Mahajan, professor of surgery, has uncovered a novel epigenetic mechanism that causes prostate cancer to become castrate-resistant and has developed a new androgen receptor antagonist that can suppress prostate cancer growth. Kiran Mahajan, assistant professor of surgery, is targeting epigenetic regulators in metastatic castrate-resistant prostate cancer.